Low AMH levels? Regain hope and control of your fertility
Understand low AMH, its impact on fertility and treatment options. Find out how to improve egg quality and increase your chances of conception.
A fertility test is not just a biological evaluation, but a long journey towards the coveted joy of conception, combining emotions, timing and science.
"The lab results are back, but I don't understand a word!" You're not alone. Many people leave the lab clutching their fertility test reports in despair, with no idea what the numbers mean. When conception doesn't happen as expected, many couples turn to fertility testing for answers.
Fertility testing isn't just about the numbers; it tells the full story of how patients' bodies work, their reproductive potential and the obstacles that stand in their way.
Whether you're preparing for pregnancy, considering assisted reproduction options or simply curious about your fertility, understanding the parameters of a female fertility test and a male fertility test will help you regain control of the situation and engage in constructive discussions with healthcare professionals to define the way forward.
Fertility testing in women involves imaging studies, hormonal assessments and cycle monitoring. For male fertility testing, semen analysis or "sperm count testing" is the main examination.
These tests don't determine a person's worth, they don't definitively establish their chances, and they don't write the final chapter of their hopes.
A fertility test is a guide, a chapter in a larger story - a story of truth.
In this section, we'll highlight the most essential indicators and parameters of fertility testing in women. Continue reading :
Anti-mullerian hormone, or AMH, is produced and secreted by the granulosa cells of the pre-antral and small antral follicles (2 to 10 mm) of the ovaries. It indicates ovarian response potential, particularly during processes such as IVF (in vitro fertilization).
To put it simply: if your ovary is a factory, AMH is like the gauge that indicates "the machine is ready to go".
Age, lifestyle and hormonal balance play an equally decisive role, which is why AMH must always be interpreted in a more global clinical context.
If you're 35 or under and have a low ovarian reserve, your age may be your greatest ally. Oocyte quality often compensates for a lower quantity, keeping your chances of conceiving naturally higher.
Follicle-stimulating hormone, or FSH, is secreted by the pituitary gland and triggers the development of follicles in the ovaries. When the ovarian reserve diminishes, the body compensates by secreting more FSH. This means that HIGH FSH levels indicate reduced fertility potential.
Consistently high FSH levels can make conception more difficult, but this does NOT make pregnancy impossible; couples can still conceive through assisted reproduction or with medical support.
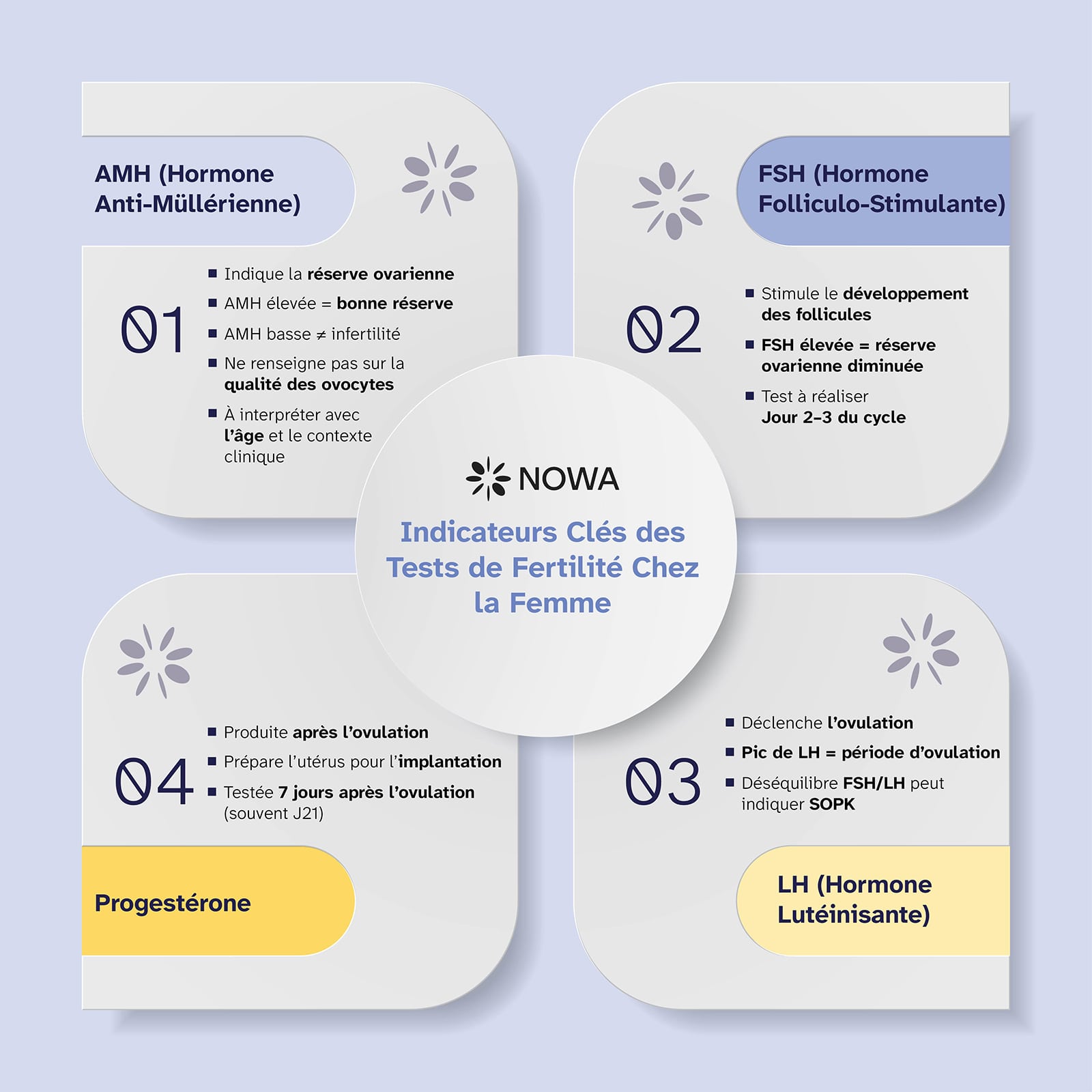
Luteinizing hormone, or LH, peaks in the middle of the cycle to trigger ovulation, i.e. the release of a mature oocyte.
An imbalance between FSH and LH may indicate the presence of hormonal disorders or PCOS (polycystic ovary syndrome), which disrupts the regularity of menstrual cycles.
The two hormones are like the melody and rhythm of the cycle:
one stimulates growth and the other synchronizes release.
Progesterone is secreted by the corpus luteum after ovulation.
This hormone thickens the uterine wall to prepare it for implantation.
A progesterone test performed around cycle day 21ᵉ, or 7 days after ovulation, confirms whether ovulation has occurred or not.
Progesterone is often referred to as the "pregnancy hormone".
It is essential not only for conception, but also for maintaining an early and healthy pregnancy. Repeated miscarriages early in pregnancy can sometimes be linked to insufficient progesterone production.
In this section, we highlight the complementary health assessments that complete the overall fertility assessment.
Pelvic ultrasound is considered to be one of the best examinations for fertility testing in women.
It assesses the antral follicle count (AFC), i.e. the number of small follicles visible in the ovaries at the very beginning of the menstrual cycle.
A healthy AFC supports a good ovarian response during fertility treatments such as IVF or even during natural cycles.
Infertility is not just a female problem. In 40% of cases, the cause is linked to male factors.
The male fertility test, also called spermogram, evaluates :
Men are advised to avoid ejaculation for at least 3-5 days before a fertility test, as well as avoiding exposure to excessive heat, such as working with a laptop resting on their lap, and staying well hydrated. Excessive heat temporarily reduces sperm quality, while dehydration affects sperm motility, quality and volume.
Hormones are dynamic and constantly fluctuating.
No single result can define a person as fertile or infertile - it's the repeated patterns that count.
The factors that influence hormonal variations are :
"When my doctor told me my AMH was low, I thought my dream of becoming a mother was over. She explained that one result doesn't tell the whole story - six months later, I conceived naturally." - Marie, 38 years old
Reassessing fertility indicators provides a clearer picture of how the situation is evolving. Re-testing is recommended when :
Regular monitoring helps to observe how the body responds to personalized treatments.
Once you have your results, start the discussion with your doctor or fertility specialist. Remember: your results are the start of a conversation, not a conclusion.
Questions to ask your health specialist:
Support your body holistically to increase natural conception potential. Here's how:
Key takeaways from this blog:
Fertility is a deeply personal journey, and a single test result will never define your worth as a future parent.
Behind every number on a male or female fertility test, there's a story of science, resilience and hope working on your behalf.
Surround yourself with specialists who listen to you, explain each possibility and walk alongside you with empathy,
because fertility is always a question of possibilities, much more than biology.
Personalized suggestions based on your reading and fertility goals - curated by Nowa's team and algorithm.

With a decade of experience in reproductive medicine, Dr. Maget combines clinical expertise and data-driven knowledge to help individuals and couples approach their fertility journey with confidence.
.svg)
.svg)
The results are dynamic and reflect the current state of fertility. However, parameters may fluctuate according to lifestyle, health, age, stress, medication or illness.
.svg)
.svg)
For women under 35, doctors recommend these tests when pregnancy does not occur after 12 months of testing. For women aged 35 and over, testing is recommended after 6 months of trying. Fertility tests for men should be carried out after 6 to 12 months of regular intercourse, or immediately in the presence of risk factors such as age, surgery or illness.
.svg)
.svg)
A female fertility test includes hormone analyses such as LH, FSH and AMH, as well as ultrasound of the uterus and ovaries, and sometimes fallopian tube imaging. A male fertility test is most often called a sperm analysis (spermogram), which evaluates sperm count, morphology, motility, etc. In the event of abnormalities, hormonal analyses and imaging tests may be carried out.
.svg)
.svg)
A low ovarian reserve or reduced sperm concentration can make conception more difficult, but not impossible. There are many options, both natural and assisted, depending on the case.
Discover unique information about your body with Nowa's personalized fertility test - designed by experts and accelerated by our technology.
Do the testTake the NOWA fertility test to find out in just 3 days.
Do the test

Choosing an assisted reproductive technology clinic abroad can quickly become confusing. Criteria, pitfalls to avoid, personalized approaches: we help you see clearly and make a choice that is right for your situation.

Understand low AMH, its impact on fertility and treatment options. Find out how to improve egg quality and increase your chances of conception.
A fertility test is not just a biological evaluation, but a long journey towards the coveted joy of conception, combining emotions, timing and science.